Plantar Fasciitis (Plantar Heel Pain)- A Complete Guide based on Research Guidelines
What is Plantar Fasciitis? A Modern Definition
Plantar fasciitis is the most common form of disabling foot pain. In fact, it is so common, that it affects somewhere between 4% to 7% of our communities. It is experienced primarily as a pain in the heel region, and is at its worst with the first steps when getting up in the morning, or after having rested for a while during the day. It most common in two groups of people - middle age and older adults, as well as runners.
The plantar fascia thick band of tissue that runs along the arch of your feet from your heel to your toes and aids in stabilization of your arch while you walk, run, and do other weight bearing activities. Plantar fasciitis was historically thought to be an inflammation of that tissue. However, in the last 20 years we have discovered that there is actually very little inflammation involved (although their may be some). The tissue actually becomes disorganized and degenerative (although not irrecoverable). It is now felt that the best terminology is actually ‘plantar heel pain’. Plantar fasciitis, however, has become the term commonly known to most people so we will use the terms interchangeably in this webpage.
Do you want a quick summary of this information? See our Plantar Fasciitis Quick Guide.
E3 Rehab reviews some of the myths surrounding plantar fasciitis in this very informative video here, and in doing so give you a lot of great information on what plantar fasciitis actually is. This video sets the stage nicely for the guidelines that we will be recommending in this guide.
The BJSM Management of Plantar Heel Pain Best Practice Guide - Overview
With the modern definition in mind, the British Journal of Sports Medicine (BJSM - a division of the British Medical Journal) recently published an excellent Best Practice Guide for Plantar Heel Pain. Many previous guides have used low quality evidence and a kind of ‘shotgun approach’, recommending all sorts of different interventions, but not teasing out the best “bang for your buck” treatments - the ones that are most likely to help and have the highest quality evidence.
Using the evidence from high quality systematic reviews, previous guidelines, expert opinion, and patient feedback, the researchers were able to develop an high quality evidence-based management approach to plantar heel pain with very specific recommendations. We believe this is the best approach to plantar heel pain. Our approach is to use this framework, and then put the ‘meat’ on it that gives you the practical, contextual information you need to follow it.
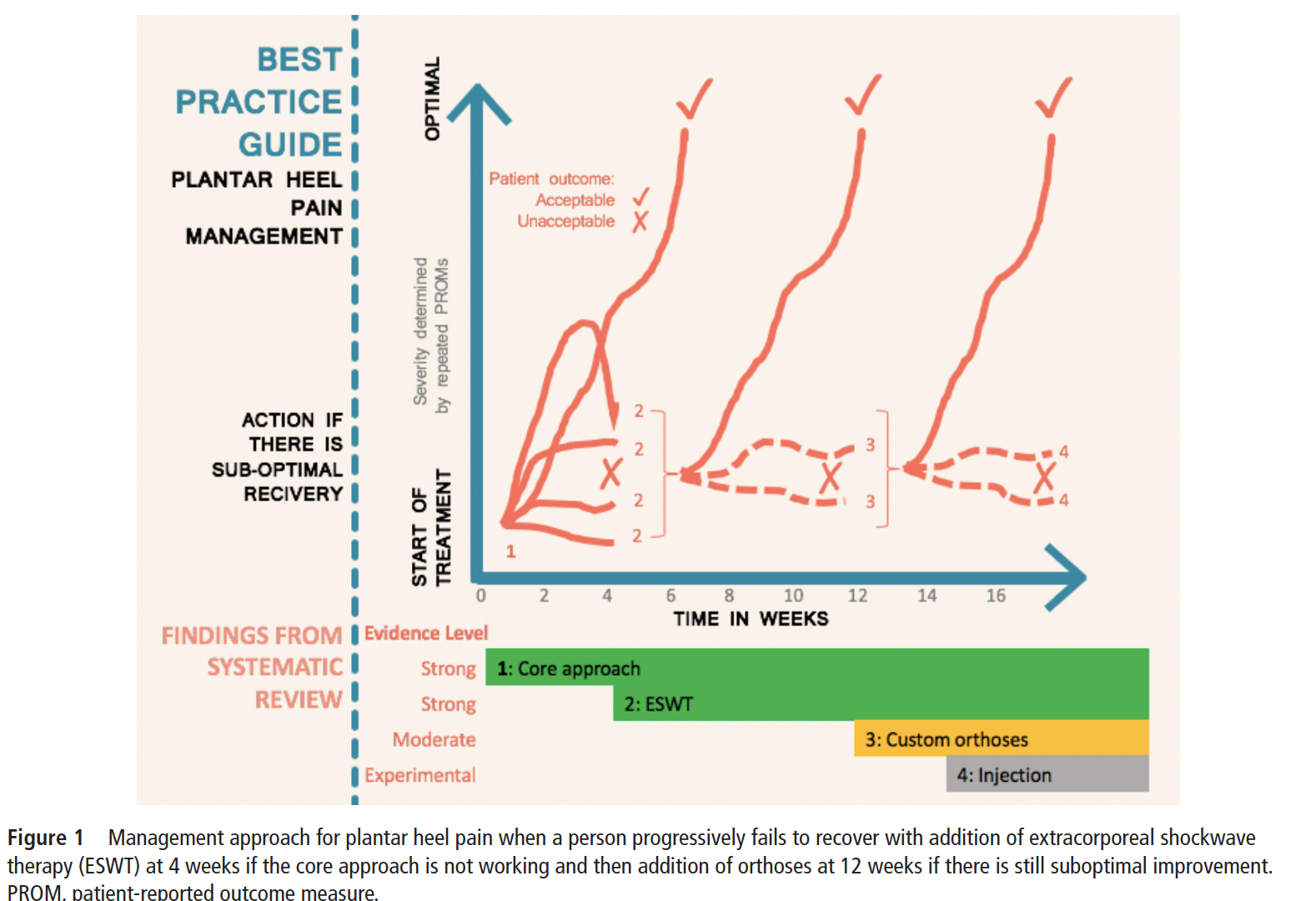
The BJSM Guidelines follow a step-wise approach, based on a timeline of treatment. There are 4 steps. At the end of each step, a certain number of people with the condition will find their heel pain is resolved. If it is not, then they should proceed to the next step of treatment.
This approach can be outlined as below. Click on each step to get more details outlining the appraoch.
-
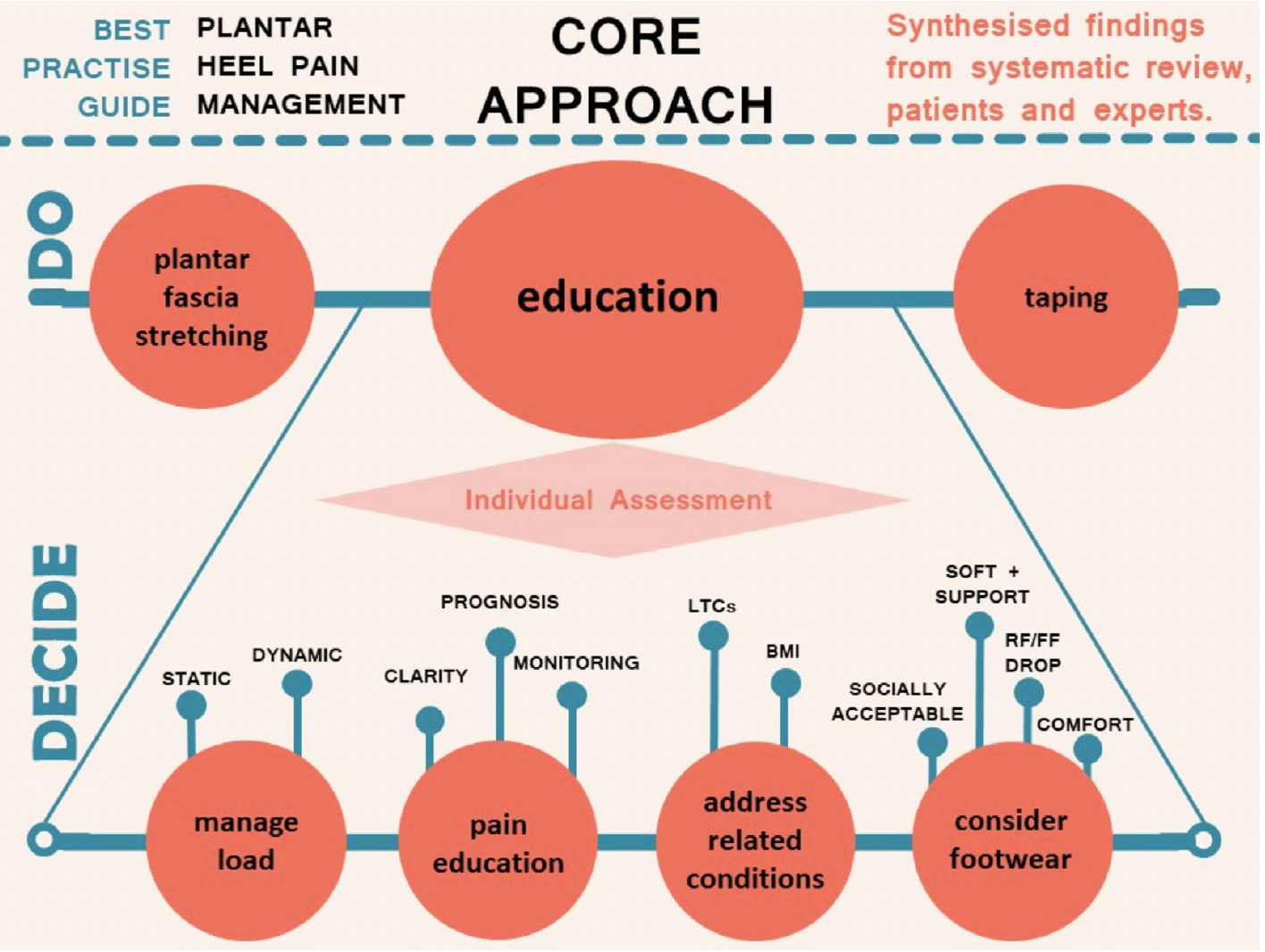
The CORE treatments for plantar fasciitis include plantar fascia stretches, taping, and education. Stretching and Taping can be applied universally, while the education required will depend on the lifestyle and characteristics of the individual patient. The goal of this guide is largely to give you the practical CORE treatment and the education required to manage plantar heel pain.
-
Extracorporeal Shockwave Therapy (ESWT) should is recommended if the CORE treatment approach has not resolved the plantar heel pain by 4 weeks. ESWT will need to be applied by an experienced physiotherapist and is typically recommended for 3-5 sessions over 4-8 weeks.
-
If after ESWT the condition continues to persist, custom orthoses are recommended. Some clients may be able to manage wtih just prefabricated orthoses. FusionPhysio has physiotherapists experienced in lower extremity biomechanical assessment can make orthoses recommendations as well as prescribe and order custom orthoses for you.
-
After 8 to 12 weeks of the above treatment, some cases of plantar fasciitis may still not be resolved for various reasons. In these cases, adjunct interventions are recommended based on the strength of the quantitative evidence and expert reasoning. Although, a return to the CORE approach ensuring greater adherence and accuracy may also be recommended.
The diagram below gives a visual representation of the timeline of this stepwise treatment, as well as an indication of the evidence levels for each step of the approach.
A qualifier for the BC Health Care System . . .
In reality, with the delays of our health care system, by the time we see our doctor and / or make it into a physiotherapy appointment , many people are 2-3 months or longer into dealing with the condition. Or in some cases, individuals make take several months before they decide to get help. In the case of a condition that has already been ongoing for sometime, is recurrent, or shows a very definitely biomechanical presentation, the timeline of steps may be moved up or recommended together in order to expedite recovery.
Step 1: CORE Approach
The CORE approach is the place to start your plantar fasciitis treatment. It has 3 components. The first two components can be started right now. The third component may require professional assessment and review to determine which factors are most relevant to your condition.
Step 1A: Plantar Fascia Stretching (DO) - Everyone with plantar fasciitis should do stretching of the plantar fascia. Stretching for plantar fascia is both safe and effective. We provide the most effective plantar fascia stretch as well as related calf stretches below.
Step 1B: Plantar Fascia Taping (DO) - Everyone with plantar fasciitis should use taping to reduce their symptoms. Taping supports the arch and minimizes plantar fascia strain during weight bearing activities.
Step 1C: Education (DECIDE) - Beyond stretching and taping, there are a number of other things that you can help assist in managing and resolving plantar fasciitis. Whether these apply to you will depend on your specific lifestyle and body characteristics. These items are covered below, but a professional assessment may be very useful for helping identify which of these are most relevant to address and how best to address them.
Step 1A: Plantar Fascia Stretching (Do - For Everybody)
Plantar Fascia Stretching (Direct Plantar Fascia Stretch)
There are many exercises you can find online for plantar fasciitis, however, there is one stretch that has a high level of evidence. Physiotutors shows the stretch well in the following video.
The studies suggest holding the stretch for 10 seconds, repeating 10 times, and performing this 3 times per day. While ideally this is what you should do, many people will find it hard to be successful with that amount of stretching. However, even completing partial amounts of the recommendation will be beneficial.
Calf Stretching (Indirect Plantar Fascia Stretch)
As we age, our calf muscles often get tighter, and tight calfs can contribute to additional plantar fascia strain. We frequently find calf stretching is beneficial to those with plantar fasciitis by indirectly allowing more plantar fascia flexibility.
There are many types of calf stretching, but this is one of the most common. Hold this stretch for 30 seconds, and perform it 2 times in a row. Do it two times per day. Calf stretching can also be done with a slant board (see Pro Tip below)
Step 1B: Plantar Fascia Taping (Do - For Everybody)
Plantar Fascia Taping
Many different versions of plantar fascia taping can be done. To be effective, taping should be fairly simple, durable and able to be applied at home. This video, using a leukoplast tape, shows one of the most effective versions that is simple enough to be done at home. You will likely need some assistance in applying the tape.
With any taping, you should be sure you don’t have allergies to tapes and monitor your skin closely to ensure it is handling the intensity tape glue. If you need a little more help in getting started with plantar fascia taping, book an appointment for us to show you how to apply it yourself.
PRO TIP: Daily calf stretching can help many foot / ankle conditions, but many people have trouble remembering to do it. A quick memory aid to remember your calf stretching 2x daily is to put a slant board or foam roll wedge by your bathroom sink and stretch your calfs while brushing your teeth!
Step 1C: EDUCATION (Decide - Individualized Recommendations)
While the “DO” section includes items that are universal to all patients with plantar fasciitis and in some cases may be all that is needed, the DECIDE section requires individual assessment as to which items are relevant to you. The relevance of the following items are best assessed by one of our experienced physiotherapists to determine the relevance to your particular plantar fasciitis. Where relevant, we expand on the
Manage the Load
For tissue to heal, we must allow the load we put on it to match its capacity to withstand that load. The load is the tension and pressure that goes through our fascia as we do weight-bearing activities. In order to heal, we must therefore decrease the load on the plantar fascia, or, increase the capacity of the plantar fascia to withstand load, or both (of course, this is the best . E3 Rehab explains this concept well in this video.
Decreasing the Load
Activity Modification - ‘modification’ is the key. If at all possible, we do not want you to stop your exercise, however, you may need to reduce it temporarily. After assessment, we can work with you to establish an activity modification plan
Prefabricated Orthotics - If taping is highly successful, you may wish to consider a prefabricated orthotic as a part of the CORE approach, as an orthotics has a similar effect on tissue tension
Custom Orthotics - if taping works, then typically custom orthotics will work as well. Orthotics decrease the tension through the fascia by reducing the flattening of the arch (overpronation) and raising the heel. The may also act as a shock absorber. The main reason custom orthotics are not introduced earlier in the treatment recommendations from the BJSM Guidelines is due to the cost of scanning, prescription, and fabrication. However, in cases of obvious biomechanical faults, overweight / obese patients, protracted plantar fasciitis, or recurrent symptoms over time, they may be recommended earlier.
Footwear - the construction of footwear can also have a significant effect on the plantar fascial strain. Many people experience an onset of plantar fasciitis after a summer of wearing zero support flip-flops. Some footwear actually increases the strain on the plantar fascia, by lowering the heel in cushioned material.
Weight Loss - While extremely important and a high predictor of plantar fasciitis, this is probably the most difficult of the Load factors for people who need it to modify. There are not many people who need to lose weight, who don’t know that losing weight would be good for them in all sorts of ways. It’s not the knowledge that is the problem, it’s how to do it. Sustained weight loss doesn’t just require a small change here and there, it often involves lifestyle change that takes commitment, accountability, time, and usually some help. Although we have our own thoughts on the strategies we have seen help the most, we defer to the experts in this area and provide links for help with weight loss here.
Walking Boots - rarely do those with plantar fasciitis need to go into a walking boot, although in extreme cases it may be recommended. One should only start using a walking boot under the guidance of a healthcare professional (doctor or physiotherapist), temporarily, and with a clear plan to wean off use after several weeks.
Increasing the Capacity
There is one main way to increase the capacity of the plantar fascia and that is through exercise. The exercise protocol in the video to the right continues to be the most accepted way to increase plantar fascia capacity.
This exercise causes heavy loads across the degenerated tissue and stimulates healing. The exercise actually has better results than daily plantar fascia stretching. Of course, you would do best to do both exercises.
Although it is ok to feel some pain. with this exercise, you should start it with caution and you may need to work with a physiotherapist to find the most appropriate starting load level
Use Appropriate Footwear - As Much As Possible!
Wearing proper footwear is critical to plantar fasciitis healing. While many people resort to soft sole shoes to reduce the pain of contact, providing stability and support to the foot is more important to preventing strain and allowing for actual healing of the tissue. Most people should be wearing stable shoes that reduce the pronation of their feet. We have seen great success with the Brooks Addiction Running shoe, Brooks Addiction Walking Shoe.
When you start to treat your plantar fasciitis, you should try to wear supportive shoes whenever you are on your feet (both inside and outside) for at least several weeks. Ideally, this would mean wearing your shoes inside the house, but a supportive sandal would also be acceptable. This means keeping shoes/sandals beside your bed to put on as soon as you get up in the morning. Avoid going
The BJSM Guidelines emphasize that footwear must not only have stability, but also be comfortable and socially acceptable to actually be consistently worn. You will need to make the decisions on comfort and style for yourself, of course. To help you with footwear choices, you can link to our footwear guide developed from podiatrist recommendations. The footwear guide has a great variety of choices and using it, you should be able to find footwear that meets all of these criteria.
Address Related Conditions
Conditions Altering Healing and Weightbearing
Other conditions can affect healing and tissue load and should be taken into account when setting expectations on healing rate. Chronic conditions such as diabetes should be kept as well controlled as possible with the assistance of your family physician. Any wounds or surface conditions of your feet that cause altered weight bearing and gait patterns should be taken care of with a foot care nurse or podiatrist.
Weight Loss
As can be guessed, excessive weight increases tissue load on the plantar fascia and makes it harder for plantar fasciitis to recover. As previously mentioned, losing weight requires a committed lifestyle change and this may be your opportunity to do be inspired to take this change on. The video from Dr. Huppin
Understand the Pain (and Prognosis)
Prognosis
While the prognosis for plantar heel pain is positive (in most cases it is likely to resolve with time and treatment), It is important to understand that it will likely take some time to do so. Usually we are talking months rather than weeks. As such, it is important to be committed to the recommendations of the CORE program and realize that you should not abandon the measures if the symptoms do not resolve immediately.
Pain Monitoring
It is important to monitor your pain levels in response to your activities, exercises, and footwear choices. Progressively increasing pain over several days typically means the load being applied to the plantar fascia is exceeding its capacity and healing is not taking place. For resisted exercises, guidance in allowable pain may be necessary. Use our Traffic Light Pain Monitoring Guide to assist you in determining reasonable levels of pain with exercise. As a bottom line, it is ok to feel slight pain during the exercises, but not after the exercise and you should not have increasing pain the next day.
Step 2: Extracorporeal Shockwave Therapy (ESWT)
The CORE approach should be undertaken for 4-6 weeks to establish effectiveness and determine baseline pain levels. If your condition is still unresolved, Extracorporeal Shockwave Therapy is recommended. ESWT requires 3-5 treatments, typically on a one treatment per week schedule. You can contact us to book an appointment for Plantar Fasciitis ESWT.
Step 3: Custom Orthotics
If after a course of shockwave therapy your condition is still not significantly improved, the guidelines recommend using custom orthotics. These may also be recommended earlier in the process if certain biomechanical faults are noted, you have a history of recurrent plantar fasciitis, or struggle with your weight.
Many Extended Health Benefit Plans provide coverage for custom orthotics. Call your plans customer service line to determine if you are covered.
Custom orthotics will typically require an assessment and casting (plaster, foam, or laser scan cast). In some cases, we can provide. Many plans will allow FusionPhysio to make your orthotics for you. Other plans, however, will require you to see a podiatrist, orthotist, or pedorthist.
Step 4: Consider Evolving / Lower Evidence Treatments
Other options have been reported as potentially effective for plantar fasciitis when the above options fail, but the evidence as uncovered by the BJSM Guidelines was insufficient to meet the criteria for recommendation as Best Pratice
Patients who are still unresolved after Step 3 may which to return to the CORE treatment with greater adherence and give the condition more time, or may which to try evolving treatments such as injection or dry needling that have yet to show sufficient evidence for clear recommendation to see how these work for them. Discussion this with your healthcare professional is recommended